The COVID-19 pandemic disrupted health care around the world, including efforts by URC projects to reduce the spread and human impact of tuberculosis (TB) and its drug-resistant strains. Mandatory transportation shutdowns, curfews, and social distancing measures – particularly early in the pandemic – created a significant hurdle for our projects to achieve their goals in support of national TB targets.
However, URC TB-focused projects in Uganda, the Philippines, South Africa, and elsewhere quickly adjusted to these new realities. Working with government counterparts, these projects devised innovative ways to identify TB cases, connect patients to effective treatment, train health care providers, and carry out communication and behavior change activities.
“Tuberculosis does not self-quarantine,” said Carlos Cuéllar, URC Executive Vice President for Technical Programs. “Therefore, we at URC adapted our service delivery models to reduce face-to-face contact and increase community-based TB outreach and treatment, for example.”
URC’s Global TB Experience, Expertise
Guided by science and the appetite for innovations, URC has an extensive history in TB programs, both in their global reach and achievements. Since 1990, URC-led programs have addressed TB in more than 24 countries – including 11 World Health Organization high-TB burden countries – and worked in all 10 USAID National Action Plan MDR-TB countries.
URC has implemented large, multi-country, USAID-funded projects to tackle TB, including USAID TB Care II, the USAID Applying Science to Strengthen and Improve Systems (ASSIST) Project, and the USAID Translating Research into Action (TRAction) Project. And we have developed technology and approaches that have contributed to a 20% reduction in global TB cases between 2015 and 2020. These include:
- The FAST approach, an infection control strategy for health facilities in high-TB burden countries. FAST, or Find cases Actively, Separate safely, and Treat effectively, is an administrative infection control intervention based on universal screening for TB symptoms in facilities to find and rapidly diagnose people with TB and DR-TB. TB CARE II worked with the National Tuberculosis Programs in Bangladesh, Malawi, and Vietnam to pilot and refine the approach and Vietnam adopted FAST as national policy in 2017. TBSAP implemented FAST in over 80 facilities in South Africa.
- ConnecTB, a web/mobile-based platform that allows: TB program administrators to assign observed therapy (DOT) providers to patients; DOT providers to record and report patient data during support visits, retention in TB care, home infection control measures, and ensure contact tracing is completed, among other tasks; patient geo-tagging to identify TB hot spots. URC first implemented ConnecTB in South Africa in 2015.
- The MDR-TB patient-centered care package, implemented in treatment sites. The package includes efforts to: maximize physical comfort, safety, and wellness of patients, such as through nutrition support and monitoring and treatment of drug side effects; provide psycho-emotional support, including protection from discrimination; and reduce families’ financial burden through transport assistance. URC began piloting this package in three districts in South Africa in 2016, and concluded that it helped reduce treatment time and increase adherence, among other benefits.
Bringing TB Services Closer to Patients
As transport closures and curfews limited people’s ability to visit health facilities during the pandemic, meeting people where they were became increasingly important.
In Uganda, three URC-implemented projects negotiated with the government to receive a special exemption from the country’s transport ban early in the pandemic. The USAID Defeat TB Project was able to use 10 project vehicles to deliver TB drugs to all diagnostic and treatment sites and to homes of multidrug-resistant TB (MDR-TB) in the urban districts of Kampala, Wakiso, and Mukono.
The USAID Regional Health Integration to Enhance Services- North, Acholi (RHITES-N, Acholi) Activity in Northern Uganda established COVID-19 district task forces and used project vehicles to deliver TB drugs to patients at home and to community drug distribution points, which support HIV/TB co-infected clients. The RHITES-N, Acholi vehicles also transported district tuberculosis and leprosy supervisors and district laboratory focal persons to conduct community TB surveillance and index contact tracing plus COVID-19 daily community surveillance.
And the Department of Defense HIV/AIDS Prevention Program Uganda (DoD Uganda URC Project) ensured continuation of TB treatment by requesting for movement permits from the UPDF Directorate of HIV and AIDS and working with the military to reach and refill all previously identified TB patients on treatment. While conducting the home deliveries, the project also collected sputum samples from any presumptive TB cases.
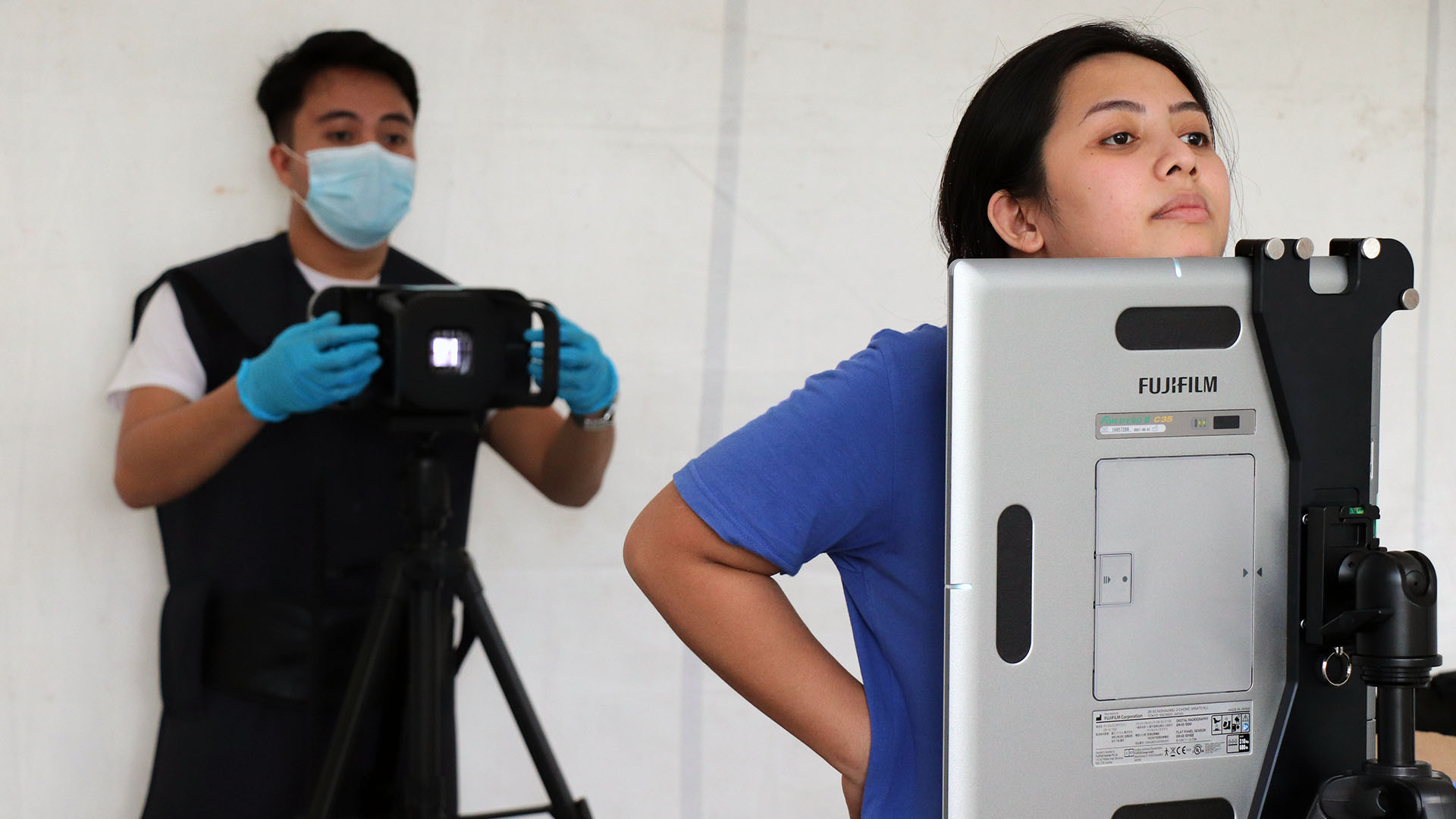
In the Philippines, USAID’s TB Platforms Project has been supporting alternative drug delivery strategies, such as arranging community drug pick-up points, including at churches and local convenience stores, called sari-sari. TB Platforms has distributed drugs at barangay health stations and directly at patients’ homes – especially for those with drug-resistant tuberculosis (DR-TB). The project also mobilized collection and transport of sputum samples by barangay health workers.
TB Platforms forged partnerships with public and private institutions, civil society organizations, and multimedia networks to carry out community TB screening and contact tracing, patient follow-up, and raise awareness about TB. And Defeat TB in Uganda expanded community-based care to cover monthly patient clinical reviews and sputum monitoring for TB and DR-TB patients. Project staff are conducting weekly calls to all patients to support treatment adherence.
In Nelson Mandela Bay, South Africa, the Provincial Department of Health initially prohibited health care workers from visiting communities during the national lockdown. But as the lockdown extended, the department exempted health care workers trained in COVID-19 protocols. The USAID TB South Africa Project (TBSAP), in partnership with the department, trained 24 health care workers from a local non-government organization, Care Ministry. All trained workers were mobilized to support COVID-19 screening campaigns in the district, resulting in 44 referrals for TB testing. This was one of many proactive TBSAP efforts during the lockdown.

Integrating TB and COVID Testing
URC TB projects are maximizing the opportunities provided by each patient contact and preparing for a future in which COVID-19 will continue to be a threat to public health.
TBSAP in South Africa has been conducting integrated COVID-19 and TB screenings with the goal of continuing these joint screenings in health facilities as part of a recovery plan the project developed.
Similarly, the USAID Cure Tuberculosis Project (Cure Tuberculosis) in the Kyrgyz Republic – led by JSI Research & Training Institute in partnership with URC – is partnering with the National Tuberculosis Center to develop a combined COVID-19/TB diagnostic algorithm to detect cases through mobile brigades which do home-based COVID-19 testing because TB and COVID-19 share symptoms. The pilot, which began in January 2021, also will help the Ministry of Health to develop an integrated approach to the diagnosis of infectious diseases.
Initial results of this joint testing pilot are encouraging: out of 718 people tested for COVID-19 by the mobile brigades in January 2021, 39 (5%) were found to have TB symptoms. Of those 39 people, six tested positive for TB (15%), including one person with COVID-19/TB co-infection, and were started on treatment.
And TB Platforms in the Philippines designed an integrated TB-COVID algorithm that is widely used today by the cities in Metro-Manila. In Manila and San Juan cities, 3,017 people have been screened for TB and COVID using the algorithm. Of those, 500 were presumed to have TB and received further testing and 105 were found to have TB. Only 1 person tested positive for COVID-19.
Using Remote Communication Tools to Reduce Face-to-Face Contact
COVID-19 has accelerated the use of mobile phones, computers, and other modern technology to talk, meet, and exchange information remotely. The pandemic also has demanded flexibility and innovation.
The DoD Uganda URC Project provided online trainings to health workers at all Uganda People’s Defense Forces antiretroviral treatment sites. The trainings covered strengthening the existing TB infection control programs to include COVID-19 prevention and TB screening generally. The project also posted educational materials for TB and COVID-19 prevention at most health facility entry points.
TB Platforms in the Philippines – transitioning from an ongoing in-person campaign – launched the “Usapang Dibdiban” webinar series, a comprehensive discussion with local government executives – including mayors, governors, and councilors handling health committees in barangays and local government units – to make TB elimination a priority and adopt funding local TB programs. Through this platform, the project raised local funding commitments of Php 42 million (or USD $86,000) for TB services.
TB Platforms also established TB contact centers in 32 health facilities in June 2020, expanding it to nearly 70 by the end of December 2020. The centers were provided with mobile phones and airtime and the staff oriented on remote patient communication and follow up, either through patients calling in or staff calling the patients who need follow-up. Between June and December 2020, the TB clinic staff provided adherence follow-up calls for 866 patients, screened 1,200 people for TB, and completed 345 contact investigations. Similarly, RHITES-N, Acholi in Uganda provided phones with monthly airtime for facility health workers to call clients and track appointments and drug refills.
TB Platforms also supported the regional MDR-TB Advisory Committees to transition their patient review meetings from quarterly in-person to monthly virtual meetings. Likewise, Cure Tuberculosis in the Kyrgyz Republic provided technical assistance to transition these meetings online, which was found to be more efficient and safer for timely consideration of cases of DR-TB patients than the traditional in-person format.

Increasing the Resilience of Health Systems
In many cases, URC-implemented TB projects are working to return, or even expand their pre-pandemic detection and treatment results. For example, TB case notification across Uganda – supported by Defeat TB – was at 5,903 in March 2020, then dipped to 3,058 in April, but rebounded to 6,500 in July.
“COVID-19 is not a short-term global emergency that will end soon,” Cuéllar said. “It is the result of trends in population dynamics, human behavior, and ecosystems which have increased the risk of emerging infectious diseases.”
“This and future pandemics demand a re-orientation of global health strategies to be more responsive to new infectious diseases and the needs of patients,” Cuéllar said. “We will continue to use our technical expertise to strengthen country responses and support the development and maintenance of resilient systems.”