The Department of Defense HIV/AIDS Prevention Program Uganda (DoD Uganda URC Project) , implemented by URC, supports the Uganda People’s Defense Forces (UPDF) in delivering HIV services to Uganda’s military, their families, and communities near the military bases.
As part of the country’s response to the COVID-19 pandemic, access to military bases where HIV services are provided was significantly restricted. Some bases permitted only HIV clients to access the health facilities after COVID-19 screening. Others were locked down completely.
These restrictions and lockdowns posed a challenge to maintaining antiretroviral therapy (ART) services for existing patients. And health workers who live off the bases faced their own transportation issues related to the lockdowns. A rapid assessment conducted within the first two weeks of instituting the lockdown – which ran from March to July – indicated that 27% of patients were unable to access their ART services and about 35% of health workers were unable to get to their jobs on the bases.
The DoD Uganda URC Project worked with the UPDF Directorate of HIV/AIDS to implement strategies to retain patients in care and ensure continuity of services. Key strategies included creating makeshift clinics near the military bases and initiating community drug deliveries and multi-month drug dispensing.
Makeshift Clinics Close Service Gaps
For military bases that were completely locked down, the project worked with health workers to move clinic services to the nearest convenient location outside the base. This benefited clients living nearby who could walk to the health facility. The process followed these steps:
- The day before scheduled appointments, health workers retrieved patient files;
- During phone call reminders, clients were informed of the location of the service point; and
- Facilities provided clients with multi-month drug refills.

Community Drug Distribution Helps Maintain Treatment
For patients unable to walk to or find the means to reach the health facilities, the project arranged for drug delivery. Each day a health facility team identified and mapped out delivery to patients, calling the patient to arrange for a community drug delivery. A team of “expert clients” – HIV-positive clients who work closely with health workers to provide peer-to peer support services including counseling and patient follow-up – carried out drug distribution via hired motorcycles (boda bodas) or with project or UPDF vehicles. The teams developed a community tracking tool to ensure proper documentation and updating of patient records with drug delivery information to accurately document the process.
One of the expert clients used his own motorcycle and took the initiative to regularly deliver drugs to client homes. The expert client, from Kakiri, said, “I know the dangers of missing (doses of) drugs; this is why I offered to deliver medications to my colleagues in the community using my motorcycle.”
At the Rubongi ART clinic, health workers used boda boda cyclists to deliver drugs to clients. Before sending the cyclist, client consent was obtained for delivery of medications. Gradually, the project worked with health facility teams to support scale-up of the drug deliveries. All activities strictly adhered to COVID-19 guidelines, including wearing face masks and maintaining social distancing.
Multi-Month Medicine Dispensing Reduces Need for Travel
Arrangements were made to provide stable patients three- to six-month medication refills. This reduced the need for frequent clinic visits which were especially challenging due to the COVID-19 travel restrictions. To ensure all facilities had adequate stocks of medicines, The DoD Uganda URC Project conducted a rapid assessment of ARV medications and supported redistribution of medicines and emergency orders as needed between facilities.
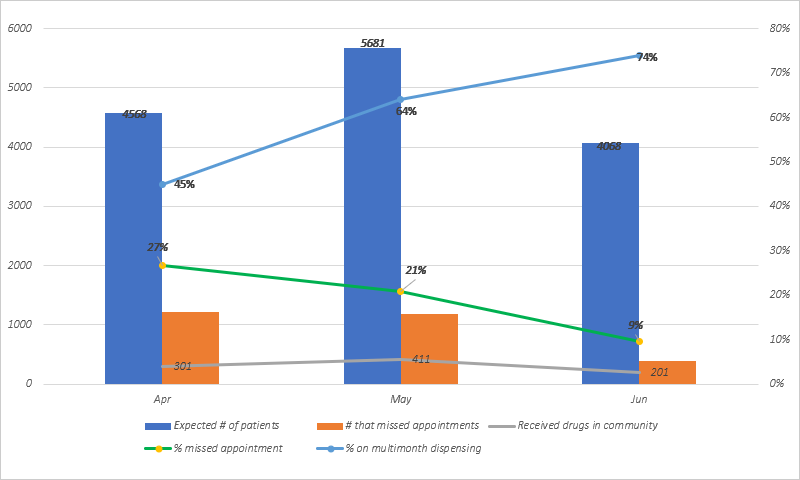
As seen in the graph below, the proportion of patients on multi-month medicine dispensing (MMD) increased from 45% in April at start of the lockdown to 74% in June 2020. At the start of the lockdown in April, about 27% of patients were missing their appointments. By June, the number declined to 9% (see figure).
Adaptations Result in Innovations
Other interventions implemented during the lockdown included community tracking of lost clients, actively referring clients to more accessible clinics, training of health workers in infection prevention, and supporting some non-resident health workers to move onto military bases to boost staffing levels and enable continuation of health services.
During lockdown, the team used telephone calls to provide intensified adherence counseling to inaccessible, non-suppressed clients. When making community drug refill deliveries, health workers took viral load samples. Non-suppressed clients who were unable to reach facilities were prioritized for community follow-up. The number of patients reached through community drug deliveries declined from May to June as the costs were high and MMD proved to be an effective, lower-cost alternative.
Overall, the combination of creation of makeshift clinics, community drug deliveries, and MMD were effective in reducing missed appointments and strengthening retention during the COVID-19 lockdown. The DoD Uganda URC Project has continued to support the UPDF to sustain MMD post-lockdown in all facilities, along with targeted use of more resource-intensive strategies, such as community drug deliveries and makeshift clinics at military bases still restricting civilian access to military facilities.
Although the COVID-19 restrictions imposed challenges, adaptations resulted in new and innovative ways to improve care and retention of clients.



