Marianne Calnan
Chief of Party, USAID TB Platforms

Abel Nkolo
Chief of Party, USAID Defeat TB
The COVID-19 pandemic halted – and likely reversed – years of progress countries were making against tuberculosis (TB). The number of TB cases diagnosed and reported globally in 2020 declined by 18%, reversing a trend of improved case detection and notification between 2017 and 2019. This likely means that more TB cases are going undetected and more people are dying from TB – the deadliest infectious disease in the world before COVID-19.
This reversal is driven by limited health system capacity to provide TB services – including health providers using testing capacity to detect COVID-19 rather than TB – coupled with a reduced willingness and ability by people to seek in-person TB services, according to the World Health Organization.
We know how to diagnose and treat TB – and can eventually end it – but we have not sufficiently harnessed the needed political will and funding to achieve this.
As TB Cases Increased, Funding Declined
As global TB cases are estimated to have increased, global spending on TB services decreased for the first time since 2016 – by $500 million, or 8.7%, to reach $5.3 billion. This is 39% of the $13 billion estimated to be required in the Stop TB Partnership’s Global Plan to End TB, 2018-2022.
Also, the Stop TB Partnership found that countries provided only $915 million in TB research funding – less than half of the $2 billion goal established by participating country governments at the 2018 United Nations High-Level Meeting on TB.
Multiple COVID-19 vaccines have been developed in record time, but only one vaccine for TB has been developed in the last 100 years. No doubt this is related to TB’s outsized impact on low- and middle- income countries, which have limited research and development capacity. The more than 1.2 million people who die from TB each year are disproportionately poor and likely to live in 30 high-burden countries.
Countries simply have not provided sufficient funding, research interest, or the political will to end TB globally.
As Dr. Lucica Ditiu, Executive Director of the Stop TB Partnership, said in a Dec. 1 statement: “It is ultimately about ensuring access for everyone, everywhere, irrespective of their vulnerabilities, and without discrimination to proper diagnosis, treatment, and care – a full package of TB services.”
But lives are being lost due to a dramatic lack of resources – especially in Africa, said Dr. Ditiu.
Despite the challenges, URC remains focused on TB treatment and prevention, especially at local levels of health systems.
Touching Lives
TB has been a primary focus of URC-implemented programs worldwide for decades. Today we work with providers, conduct implementation science, and pilot and scale up the most effective solutions for TB services.
Through USAID’s global TB CARE II Project, URC developed the Finding TB Actively, Separating safely, and Treating effectively (FAST) approach. We continue to use this approach throughout the projects we implement as we refine and bring to scale the most effective solutions for TB services. URC also applied these principles to our COVID detection and management efforts.
URC continues to be a thought leader in scalable solutions, having led TB programs for USAID and other donors in more than 24 countries, including 11 World Health Organization high-TB burden countries. From 2016 through 2019, URC led programs that detected nearly 600,000 TB cases, saved nearly 500,000 lives, and reached more than 45 million people through social and behavior change communication campaigns and other outreach.
And while COVID-19 has reversed progress on TB, URC-led TB programs have responded through adaptations and innovations, including:
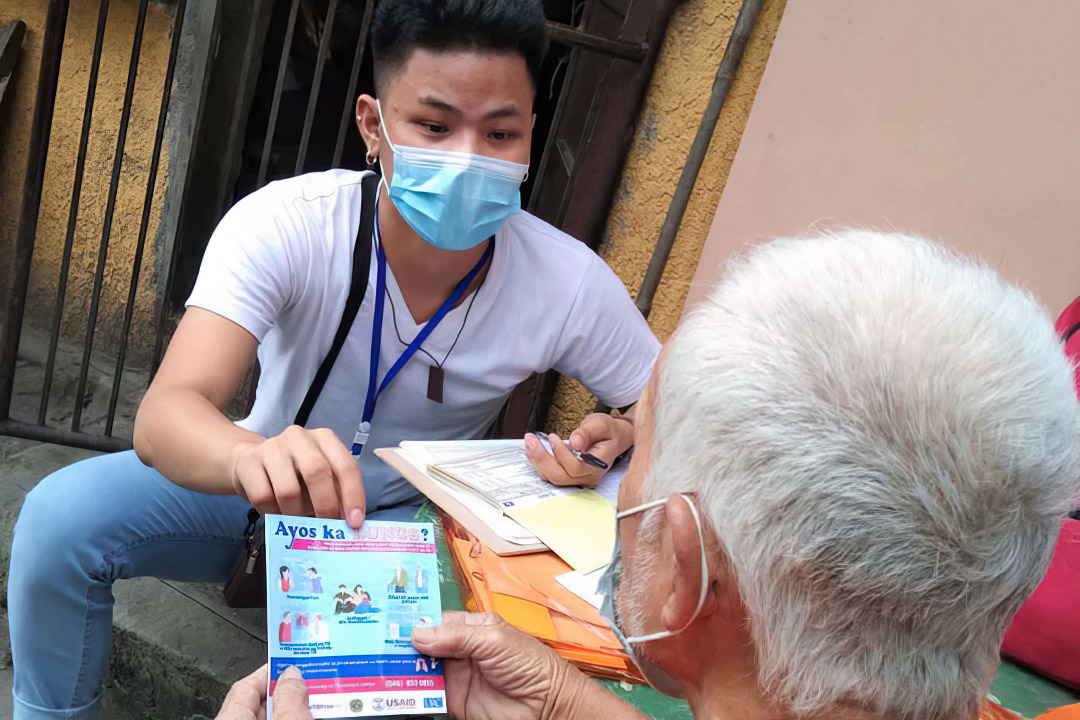
- Developing and adapting digital TB case finding and adherence tools to ensure patients had access to TB screening, follow up, and treatment adherence support.
- Scaling up health worker home visits to TB patients in Uganda and the Philippines;
- Developing a TB self-assessment form and distributing it to students and their families in the Philippines;
- Scaling up social and behavior change communication campaigns, active TB case finding, and local advocacy activities to ensure adequate funding for TB services in Uganda and the Philippines;
- Providing additional supplies of TB medicine with treatment adherence monitoring;
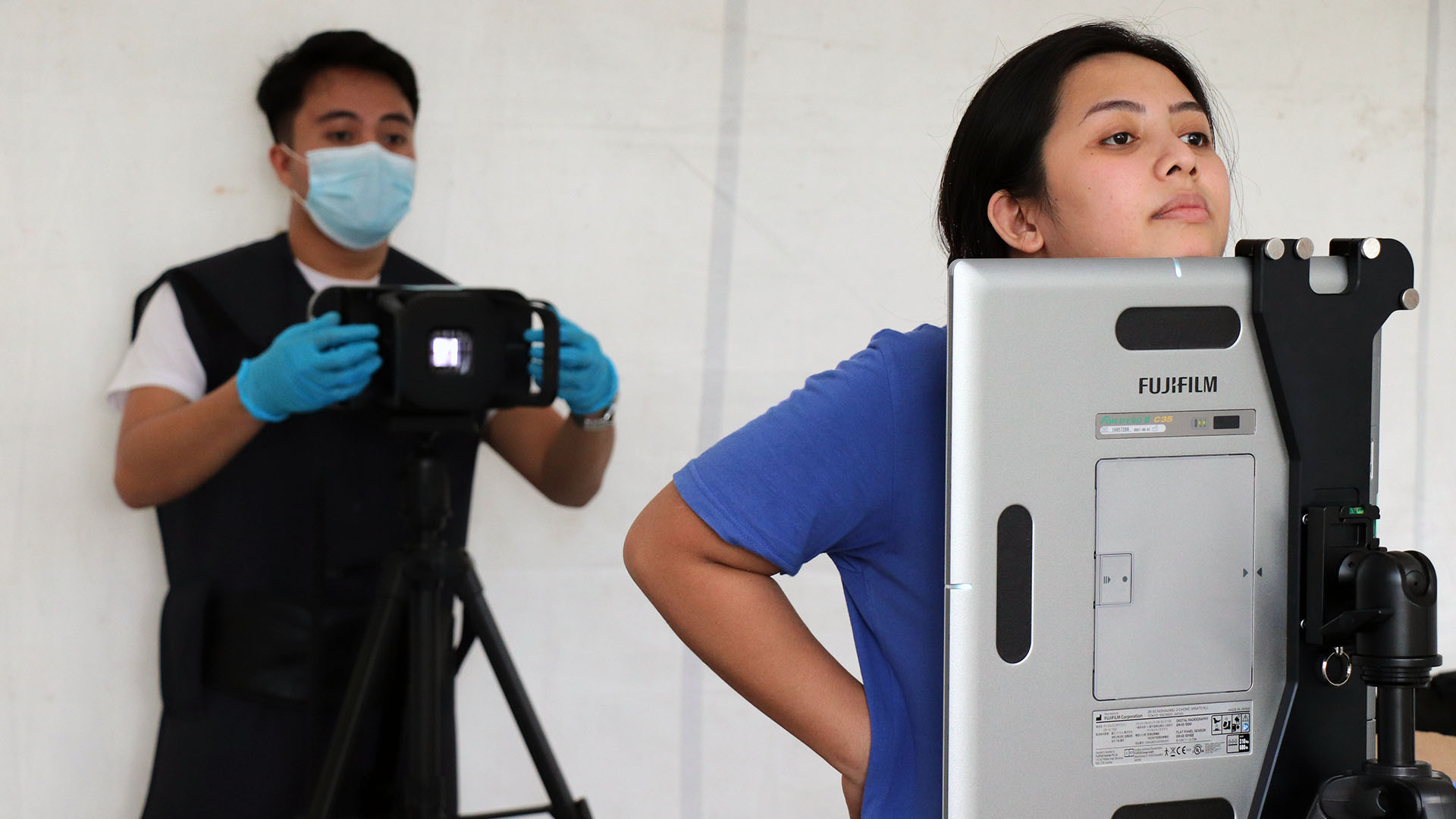
- Expanding access to TB testing by acquiring commodities and equipment and further enlisting private sector providers; and
- Training health care workers via online platforms (such as Zoom).
During the COVID-19 pandemic, we’re fighting an uphill battle against TB, but we are buoyed by the knowledge that TB is curable, preventable, and ultimately will be ended if the global community summons the appropriate resources and commitments.