Ersin Topcuoglu
Senior Portfolio Director, Asia, Middle East, & Northern Africa Programs
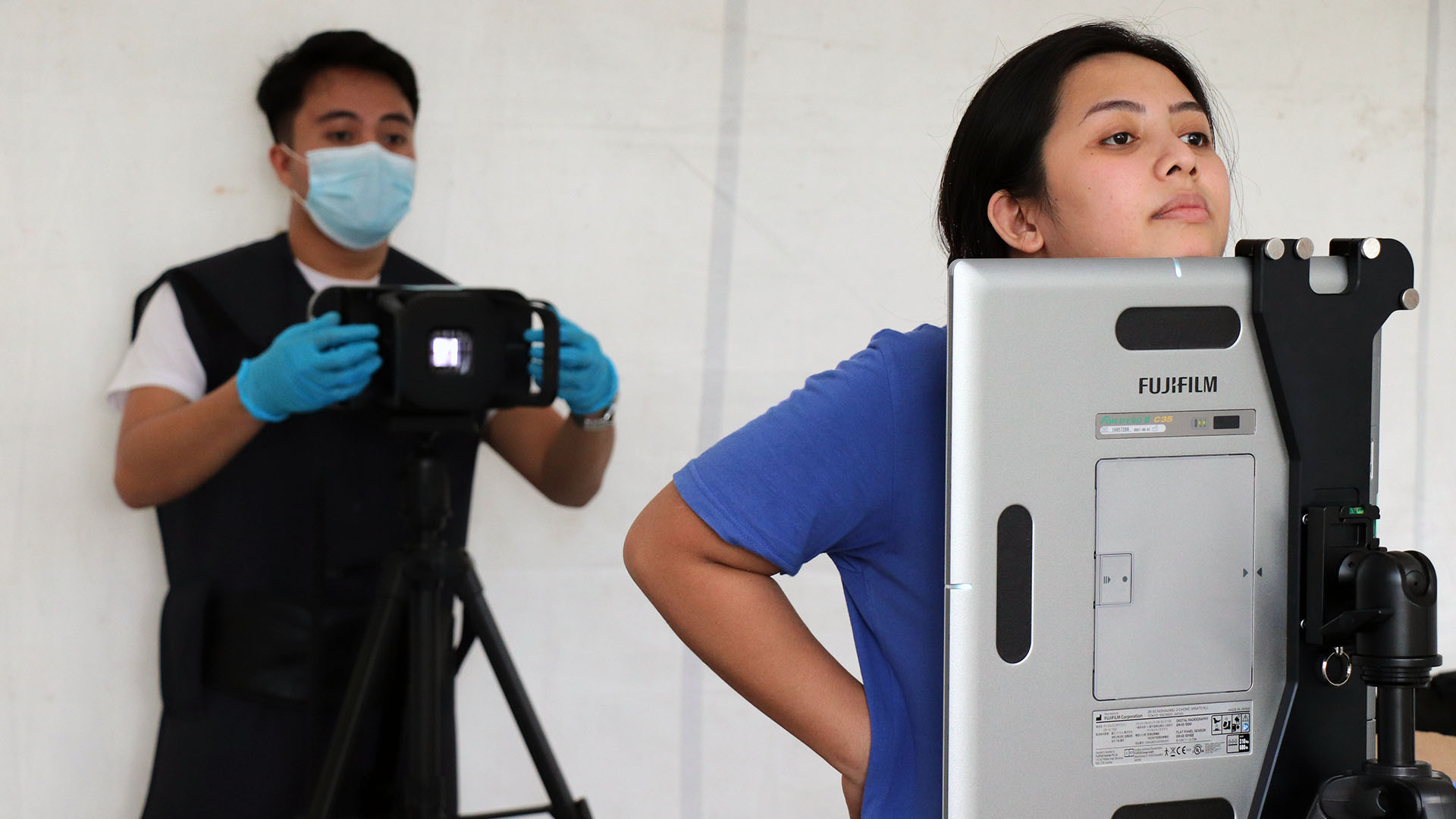
AI-driven ultraportable X-ray to increase TB detection.
Early diagnosis and treatment is the key to eliminating TB. Hope fills the global TB community when new technologies emerge to better enable screening, testing, and diagnosis in low-resource settings. But along with new opportunities comes the responsibility of ensuring best use of these technologies. This requires a lot of contextual groundwork and the application of a systems thinking approach.
Ultraportable X-ray powered by artificial intelligence (AI) using computer-aided detection (CAD) software can achieve high-sensitivity TB detection. However, there are many operational and implementation challenges.
Calibrate the Equipment
The first and most significant challenge when introducing AI-driven ultraportable X-ray for TB screening is to differentiate its diagnostic performance in community and hotspot settings with variable sensitivity.
Commercial CAD software products quantify X-ray abnormalities observed and assign these abnormalities a ranked score from 0-100. The first task for the operator introducing this technology is to select a triaging threshold score that flags presumptive TB cases. A screened patient with results at or above this score should receive rapid sputum testing using either Xpert MTB/RIF or Truenat MTB to validate their presumptive TB infection.
Choosing this score is not simply a clinical task. It’s a programmatic decision that considers and weighs various factors influencing the target population and their TB vulnerability, including demographic and epidemiologic factors, as well as varied health systems and geopolitical factors.
Adapt to Health System Constraints Ethically
When this technology is introduced, the national TB program and health system constraints must be considered. This includes the availability of quality TB treatment, patient support, and laboratory capacity for drug-sensitive and drug-resistant TB cases. Diagnosing TB patients without initiating treatment is unethical, so adequate planning and resource allocation is required to respond to an increased need for TB treatment after diagnosis as part of the continuum of care.
Finally, the national and/or regional programmatic goals and resource allocation priorities will drive the scope of any TB screening efforts powered by these novel technologies. Introducing new screening and diagnostic technologies and tools is always a political decision involving tradeoffs between investment, resource allocation, community wellbeing, and the current disease burden. This is particularly notable in low-resource settings.
Systems Thinking Key to Successful Introduction
A systems thinking approach is needed to introduce and use such novel technologies successfully. Program managers should assess how these screening efforts will trigger and affect different parts of the health system within the context of larger country-specific systems that impact health.
In a laboratory setting, a lower threshold score will lead to more presumptive patients requiring sputum testing, thus putting pressure on the laboratories, staff time, supplies, and budgets. A higher threshold, on the other hand, will put a burden on communities since missing patients will continue spreading TB and delay elimination.
We must remind ourselves that the control and elimination of TB is a product of the interaction of different parts of health systems, which are interconnected to other systems both in the country and globally that impact TB burden.
Careful consideration of the context, limitations, and impact of introducing this technology will improve the efficiency of its use and minimize harm to the health ecosystem in which it’s introduced.