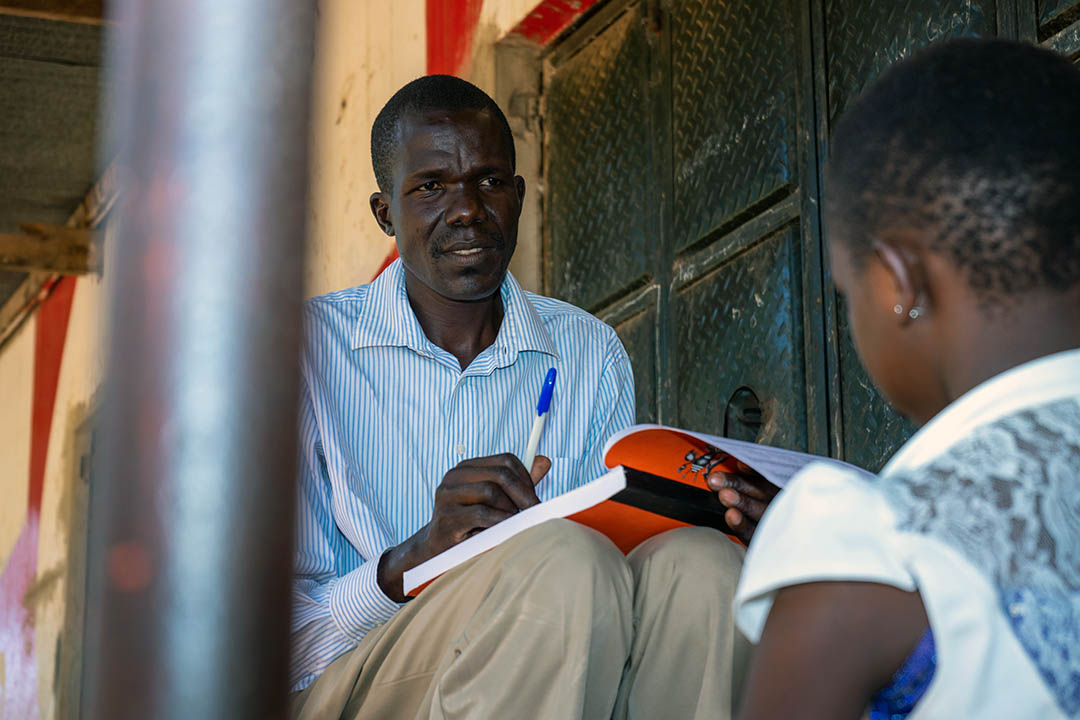
The COVID-19 pandemic compelled health care providers and patients around the world to quickly adapt to lockdowns, quarantines, and additional infection prevention protocols. In Uganda, the lockdowns affected people such as Charles Abonga, an HIV client at Nakasongola Military Hospital, who has been in HIV care since 2007.
Abonga, like other antiretroviral therapy (ART) clients, initially received treatment in the form of cotrimoxazole per the guidelines at the time. This required monthly refills and therefore, monthly health facility visits. Abonga’s wife was also receiving ART, so they would make these monthly trips to a health facility together to receive their treatment.
But when the lockdowns began in 2020, Abonga, his wife, and other clients were no longer able to make these monthly trips. So, URC – through the DoD Uganda URC Project – introduced multi-month dispensing (MMD) of ART to ensure HIV clients remained virally suppressed. This COVID-19 adaptation is part of the project’s larger efforts to achieve HIV epidemic control in Uganda in the 31 military health facilities with ART-accredited clinics, which serve members of the military, their families, and communities near the facilities.
The Benefits of Less Frequent ART Dispensing
Under MMD, clients receive between 3 to 6 months of ART drugs at each visit, depending on their viral suppression rates. And today, even after the initial COVID-19 pandemic restrictions and social distancing requirements have eased, MMD has proven to be an effective tactic to help clients maintain their ART regimens.
Viral suppression rates at military health facilities increased from 90% in July to September 2020 to 94% in October to December 2022.
MMD has become a popular option for HIV clients. Between October and December 2022, a total of 18,323 people living with HIV (PLHIV) – or 86% of people in active HIV care – received drug refills for at least 3 months, up from 35% between January and March 2020.
The Uganda Ministry of Health now recommends MMD for stable clients in World Health Organization (WHO) stage 1 or 2, who have been on their current first or second line regimen for more than 6 months, have a valid suppressed viral load, and – if TB/HIV co-infected – have completed the intensive phase of TB treatment with negative sputum smear. The prescriptions for 3 or 6 months are for clients for whom frequent drug pickups may compromise their adherence to ART.
How was MMD Implemented Successfully?
The success of MMD is due in part to its comprehensive rollout. The DoD Uganda Project team trained Uganda Peoples’ Defence Forces (UPDF) health workers on MMD protocols, provided job aids, strengthened the supply chain to ensure adequate stock, and increased community-based drug deliveries. The team supported regular onsite mentorship for health workers, tracking appointments, and increasing appointment reminders.
“Multi-month dispensing has really helped us retain our clients in care because of reduced health facility visits – they are not having to spend as much on transportation to receive their medications. This has improved appointment-keeping, and clients are happier. Certainly, the treatment outcomes have improved with reduced morbidity and mortality. Even the workload of health workers has reduced since the number of clients seen on a clinic day is reduced,” explains Dr. Mary Kiyuba, Program Officer for Care and Treatment, UPDF Directorate of HIV/AIDS.
URC worked with the military health facilities to improve MMD, tracking data at the ART clinics weekly, monthly, and quarterly through an Excel-based dashboard, and tracking monthly retention and viral suppression using the national reporting databases to identify stable clients. The project worked with health workers to provide HIV treatment and care services to clients and categorized those eligible for MMD per Uganda Ministry of Health guidelines.
Health workers determine the length of time between drug refills based on clients’ viral loads, test schedules, and other factors. For example, someone who is four months away from their next test might receive 4 months of drugs instead of 6 months, even if they qualify for a 6-month supply.
Taking Medications on Time
Abonga said MMD has helped him and his wife take their ARTs consistently. There is no longer a need for them to visit the hospital more frequently, which he said was cost-prohibitive. “People really want to take their drugs at the right time, because they know that is essential for them to be effective,” Abonga said.