James Oketch has served as a village health team member for 10 years in Kitgum District, Northern Uganda. Even as a village health team member, Oketch was wary of promoting family planning (FP) methods.
“Friends told me that a woman can over bleed and have a lot of abdominal pain if she uses family planning,” Oketch recalls. These FP myths and misconceptions are common in his community.
“People believe that the IUD causes cervical cancer or can disappear inside the uterus when inserted,” recalls Jennifer Franka Amony, an enrolled nurse attached to the Family Planning Unit at Kitgum General Hospital.
The copper intrauterine device (IUD) is a small, plastic device inserted into the uterus to prevent pregnancy. The IUD, a long-acting, reversible contraceptive method (LARC), protects against pregnancy for up to 12 years. An immediate return to fertility occurs when the IUD is removed.
Identifying Barriers to IUD Uptake
According to the most recent Uganda Demographic and Health Survey (2016), the Acholi region in northern Uganda has a high total fertility rate of 5.5 (national 5.4), a high unmet need for FP at 39% (national 28%), and a low contraceptive prevalence rate of 30% (national 39%). As of 2018, IUD uptake stood at only 1.5% in the Acholi sub-region, even though it is safe and effective.
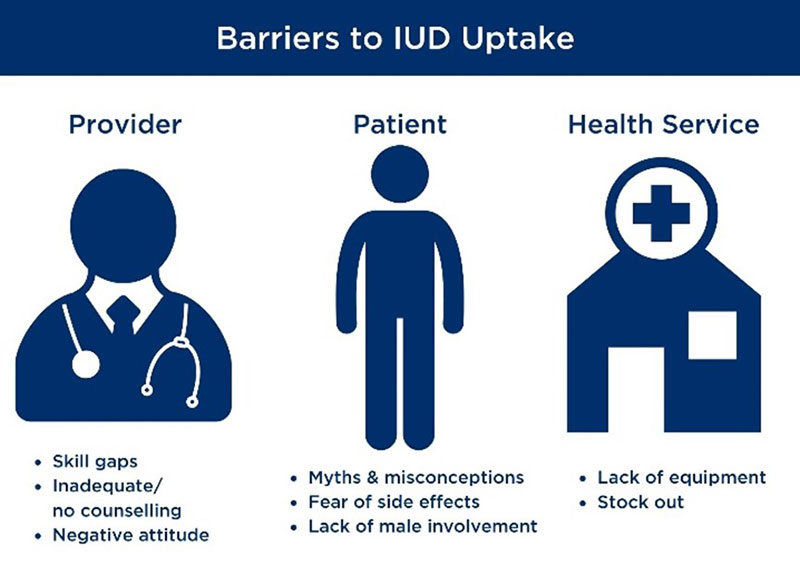
Despite the advantages of LARCs in general, and IUDs in particular, uptake of the methods have been low due to misperceptions and fears among clients, as well as barriers in service provision. URC conducted a baseline assessment in 2020 that highlighted barriers to IUD uptake (see Figure).
Making the Choice for an IUD
Akello gave birth to her second child in 2016. She weaned her older 1-year-old off breastfeeding when the baby arrived. The baby was born with sickle cell anemia. Without enough immunity, both children often fell ill.
Akello visited the health center for minor illnesses. For more complicated illnesses for herself and her family –including treatment of malnutrition requiring therapeutic feeds and for management of severe anemia requiring blood transfusion – she went to the district hospital. When the family bicycle was broken, she walked with both babies more than 12 kilometers to Kitgum General Hospital. Without enough time to tend the family garden, hunger and poverty set in, followed by malnutrition.
With things so dire, Akello went against her partner’s will and received a contraceptive injection. Her partner noticed changes in her menstrual cycle, along with side effects she was experiencing, and suspected she was using contraceptives. They quarreled and she decided to stop using injectable contraceptives.
When Akello went to deliver her third son in 2018, the couple realized the challenge of supporting three children. They feared that the next child might also suffer from sickle cell anemia. At the hospital, the health workers counseled the couple on both short- and long-term contraceptive options. She opted for the IUD, stating:
“The health workers told me about the IUD. I can now take care of my family.” And her partner, Oketch said: “We have enough food and can save enough to take our children to school. We no longer fight. Our family is happy.”
Addressing Barriers to IUD Use
The USAID Regional Health Integration to Enhance Services in Northern Uganda (RHITES-N, Acholi) Activity team worked closely with colleagues at the district management, health facility, and community levels to develop a comprehensive set of interventions to address barriers to IUD uptake.
“It’s a comprehensive approach that is important, not just one thing. We addressed all issues – provider-related, client-related, and health system-related. We placed a big emphasis on improving data quality and use – and on ensuring that we targeted lower-level facilities. We emphasized community outreach because client perceptions are critically important,” said Douglas Otoo, Family Planning Advisor, RHITES-N, Acholi.
Within a one-year period, RHITES-N, Acholi increased the total number of IUD users across the eight districts of Acholi subregion from 2,861 to 3,210. And uptake continues to improve. By the end of 2020, the Activity almost doubled the number of IUD users to 5,761.
What Strategies Worked to Improve IUD Uptake?
Targeted on-site mentorships: Quarterly targeted mentorships were provided for service providers at high-volume health facilities with the lowest IUD uptake. Topics included quality FP counseling, FP integration into routine health services, insertion and removal of IUDs, and forecasting and ordering IUD supplies.
Provision of IUD sets: RHITES-N, Acholi inventoried all FP equipment, including IUD sets, and supported the district health team to redistribute sets from overstocked health facilities to locales where they are most needed and to facilities with insufficient or no stock.
Stock management: The Activity supported district health team to track IUD sets across the districts and instituted timely redistribution efforts to avert shortages. Onsite mentorships were conducted on quantification, forecasting, and ordering adequate IUD commodities from the National Medical Store.
Strengthened IUD data management and reporting: RHITES-N, Acholi distributed new tools including a FP register and a health management information system. The FP register captures data on IUD uptake and on postpartum mothers provided with an IUD. Facility staff were mentored on use of the register and the health management information system.
Strengthened community services, linkages, and referrals for IUDs: The Activity conducted routine integrated mobile outreaches on LARCs and permanent methods at lower-level facilities and in communities in hard-to-reach areas. Trained youth peers and village health teams promoted community-based FP and served as referral agents for provision of IUDs. This created demand with clients who were referred to the nearest health facilities for IUD insertion.
Quality improvement directed towards postpartum FP: To improve IUD uptake among postpartum women within the first 12 months after delivery, quality improvement activities focused on 75 high-volume labor and delivery sites. Results show that the number of postpartum IUD users increased from 467 to 1,888 between January and August 2020. Beyond onsite skills mentorship, health workers received periodic support on data capture/use of tools, provision of guidelines, and IEC materials to continue IUD uptake.



