Ersin Topcuoglu
Senior Portfolio Director, Asia, Middle East, & Northern Africa Programs
Tuberculosis (TB) remains a global concern as the leading cause of death from a single infectious agent, ranking above HIV/AIDS. According to the 2022 WHO Global TB Report, there were an estimated 1.4 million TB deaths among HIV-negative people in 2021. The same year, an estimated 10.6 million people fell ill with TB globally.
Approximately 1 out of every 4 people are infected with TB globally. The high number of people with undiagnosed and untreated TB results in more deaths and continuous community transmission of infection, thus increasing the number of people developing TB.
Finding the Missing
There are several major challenges in finding the “missing patients” with TB infection. First, the current approach to managing TB is binomial: we manage active disease or latent infection. However, there is growing evidence that TB is a spectrum of disease states with different clinical manifestations from infection to disease. This discovery makes TB even harder to diagnose and treat. Second, there is a substantial spatial heterogeneity – or uneven patchy distribution, with clustering of cases in specific areas due to extensive transmission within communities. This means that within a single country, the incidence and prevalence of TB can have up to a 10-fold variation depending on location.

Identifying Hotspots for Targeted Mass Testing
Identifying high TB transmission settings – or hotspots – and conducting spatially targeted mass screening may help rapidly convert these hotspots to low TB transmission settings.
Such an approach will not only reduce the local TB incidence and prevalence rates but may also have a positive spillover effect by reducing the transmission from these hotspots to the neighboring communities. In low- and middle-income countries (LMICs), people living in urban slums have 3-fold higher odds of bacteriologically confirmed TB than the general population. Thus making urban slums, prisons, jails, mining company dormitories, and military barracks the default hotspots for TB transmission.
Diagnostics Delivered
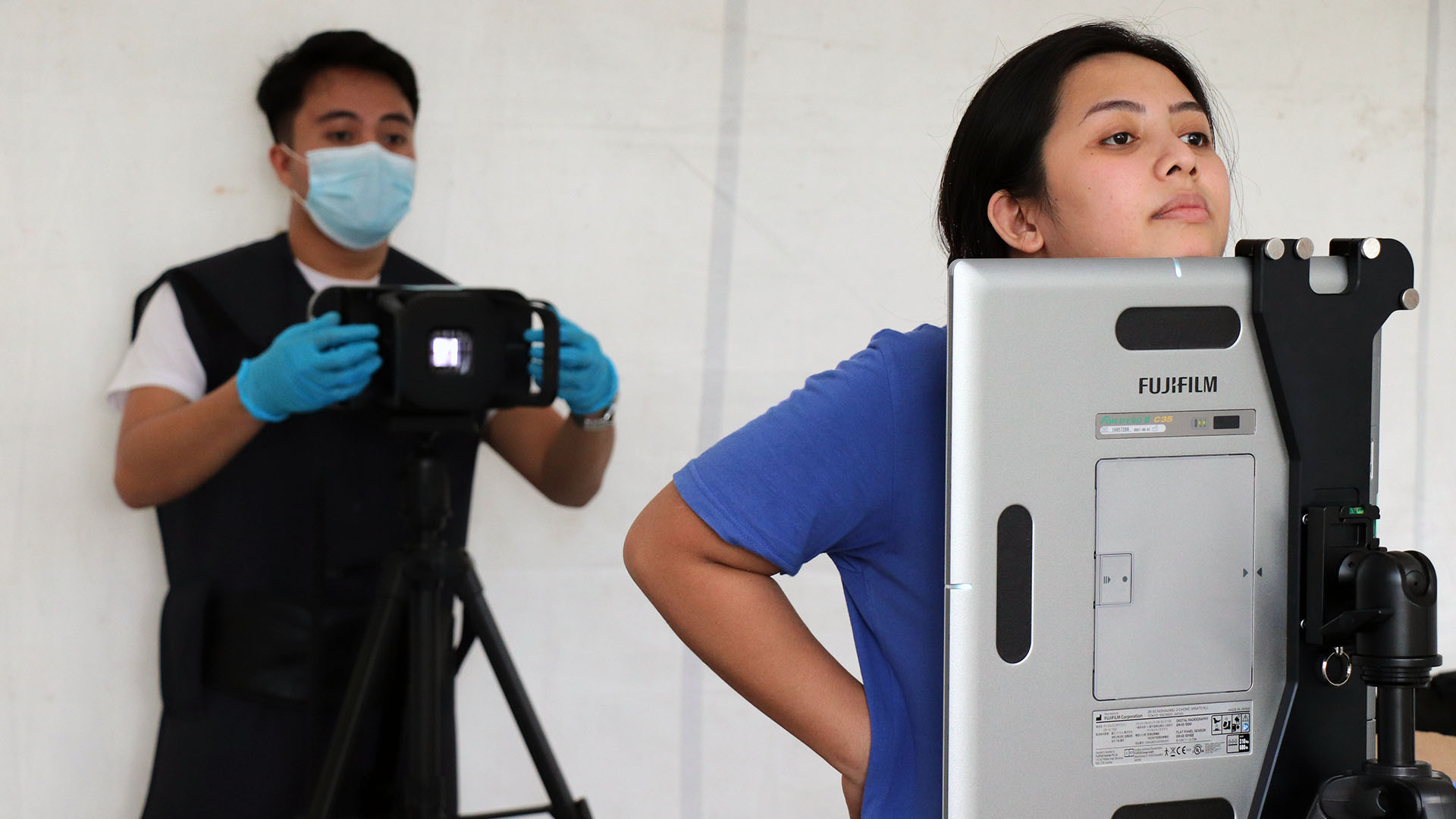
We have the tools at our disposal to test and diagnose TB in the hotspots themselves. Artificial intelligence (AI)-powered portable digital X-rays followed by on-the-spot molecular WHO-recommended rapid diagnostics (mWRD) such as Xpert MTB/RIF and Xpert MTB/RIF Ultra (Cepheid, USA), loop-mediated isothermal amplification (LAMP, Eiken Chemical, Japan) and Truenat MTB and MTB Plus tests could be ideal tools in a spatially targeted mass screening strategy.

This strategy can also help to identify patients with abnormal radiographs suggestive of active TB but with negative confirmatory bacteriological tests. Research shows that these individuals are at high risk of progressing to culture-confirmed disease with rates of progression as high as 30% to 50% over 4 to 6 years following a first abnormal radiograph. Regularly monitoring and testing these individuals with mWRDs may help to diagnose active TB earlier – and in a very cost-effective way.
Lastly, such a targeted mass screening strategy may help to reduce inequality by improving access to health care for the poor and other highly vulnerable groups, helping to avoid catastrophic costs to patients and their families.