Progress towards achieving global TB targets took a devastating hit due to the COVID-19 pandemic. Without treatment, the death rate from TB is around 50%. Coupled with TB’s infectious nature, TB prevention, screening, testing, and treatment disruptions had grave consequences.
The Pandemic’s Impact on TB Elimination Lingers, Still
Globally, many countries are still fighting their way back to pre-pandemic national TB rates. Others are coping with stalled – or worse, reversed – progress in both TB diagnosis and treatment. The number of people diagnosed with TB globally fell from 7.1 million in 2019 to 5.8 million in 2020 – a clear indicator of disconnect between the TB patient and the health care system designed to test and treat them.
Higher Burdens, Higher Stakes
The adverse impact of the pandemic on progress in the fight to end TB was especially evident in the 30 high-burden TB countries, including the Philippines. URC was two years into implementing the USAID TB Platforms Project in the three highest TB burden regions of the Philippines when the COVID-19 pandemic began: Central Luzon, Calabarzon, and the National Capital Region.
With the recent convening of the global TB community at the second UN high-level meeting on TB in New York, URC’s TB Platforms team reflected on the pre-pandemic TB situation in the Philippines at the start of the project in 2018, the bumps in the road navigated along the way, and the progress and advances achieved to date.
Proactivity Pays Dividends
Knowing the threat the pandemic posed to national TB progress, URC – together with USAID and the Philippine Department of Health – took proactive steps to maintain momentum in project activities. Of note, TB Platforms:
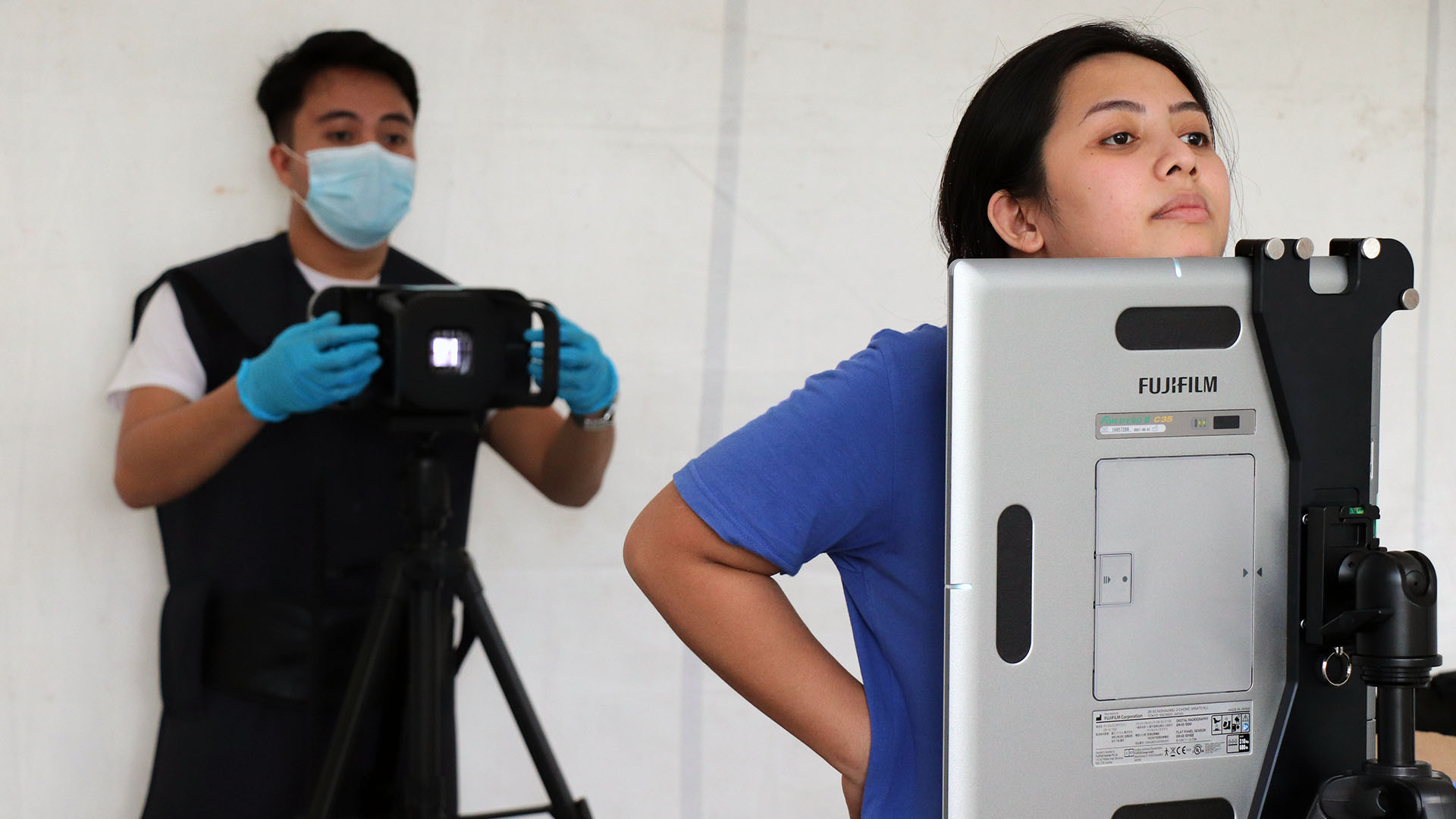
- Implemented integrated TB and COVID-19 screening and testing among at risk populations, including transport operators and the urban poor. TB Platforms screened 48,459 people with chest X-rays and diagnosed 250 people with active TB;
- Together with the Department of Education, designed and implemented “Tibay ng Dibdib,” a self-screening tool for children, who at the time were not allowed out of the homes. The self-screening tools and instructions were included in the modular learning kits distributed by the schools. The tools were also distributed during the national immunization campaign. More than 120,000 children were screened, and approximately 900 were diagnosed with TB and put on treatment;
- Strengthened infection prevention and control in health facilities using the FASTPlus strategy, whose principles and activities could be applied to reduce COVID-19 infections in the facility. It was implemented in 300 facilities which screened 2,500,000 people during 2020 and early 2021 when the community quarantines were in effect; and
- In partnership with Fujifilm, introduced the ultraportable chest X-ray with an artificial intelligence (AI) platform for reading the X-rays to reach more people with X-ray screening for TB.
URC’s Chief of Party looks back: “It was a uniquely challenging time but I know that the problem solving, dedication, and diligence of our staff and partners during the past six years, including the start of the COVID-19 pandemic, have paid dividends for years to come,” says Marianne Calnan. “We’ve already seen impressive results working with the Philippine Department of Health to defeat TB,” she continued.
To address some of the challenges in TB program delivery, TB Platforms implemented innovative strategies including:
- Fast-tracked diagnosis and treatment with FASTPlus
- Introduced new tools for diagnosis and prevention
- Strengthened climate resiliency in TB control with the SMART hospital initiative and supported disaster risk reduction and management planning in health in local government units
- Enhanced contact investigation and TB preventive treatment
- Created new partnerships to leverage resources and synergize efforts
Pride in Progress
Our efforts had a clear impact. Over 5 years of implementation, TB Platforms’ project sites have achieved more than 80% treatment coverage, improved testing rates among people presumed to have TB from 30% to more than 70%, increased the number of people receiving TB preventive therapy from 1% to 11% and increased drug-resistant TB (DR-TB) treatment success rates from 56% to 81%.
While these successes bring the supported regions closer to the goal of eliminating TB, there is still much work to be done including raising TB awareness, assuring continued resources to implement innovative solutions at scale, implementing innovations with fidelity to achieve desired outcomes, and strengthening partnerships to address the social determinants of health that the TB program can not address alone.
New Tools, Strategies, and Capacities Shine Rays of Hope
In 2021, through a partnership between USAID and the Stop TB Partnership, the introducing New Tools Project (iNTP) was initiated in the Philippines, 1 of 7 countries selected to implement this project.
The project introduced the use of:
- An ultraportable X-ray with computer-aided detection (CAD4TB) to screen people for TB;
- TruNAT, a rapid molecular based point of care test that rapidly detects active TB and drug-resistant TB; and
- 3HR, a new, shorter TB preventive treatment regimen and Digital Adherence Technologies (DAT). Specifically, the Video Observed Treatment (VOT) platform was introduced to improve TB treatment adherence.
TB Platforms implemented iNTP in 4 sites, screening 22,714 people and diagnosing 349 who were initiated on treatment over 12 months.
Using TB screening and testing as a gateway to primary health through integration with other services – such as the ‘4Ps’ program run by the Department of Social Welfare and Development, in the elementary school curriculum with the Department of Education, in workplace programs with Department of Labor and Employment, and in medical outreach services – improves health service reach and population health. Particularly in the context of the resource-constraints and social isolation of the COVID-19 pandemic.
To further extend the reach of TB services, we can continue to partner with and support community- and faith-based organizations that work in communities and settings where potential TB patients are. Building their capacities to deliver TB services and education increases the sustainability and resilience of these services through increased ownership, contextualization, and local innovation.